Articles & Podcasts
Defining Evidence-Based Orthodontics by Dr. Michael K. DeLuke https://www.orthotown.com/magazine/article/9835/defining-evidence-based-orthodontics
When Childhood Traits Become Adult Bodies – Dr Kevin Boyd & Dr David McCarty
https://www.empoweredsleepapnea.com/daves-notes/when-childhood-traits-become-adult-bodies
This one really is for everyone – Parent & Practitioners!!!
Dr Mike DeLuke’s excellent article outlining the need for a Paradigm Shift in Orthodontics. https://www.facebook.com/share/p/17viAA45Zg/
Dr Mike DeLuke’s Cleft Palate Case

Tx of a CL&P Pt w/ONLY braces & wires – NO EXPANDERS! https://www.facebook.com/share/p/1Gu67849g4/
Many of these pts have a deficient pre-Mx and, as a result, are very narrow in the anterior and middle thirds of the arch. However, the posterior third is often minimally deficient, if at all. When you use expanders in these pts, you often over-expand posteriorly and under-expand anteriorly. That’s why braces and wires are a FAR superior approach! They allow for:
Gentler forces, Differential expansion, you get expansion where you need it, Minimization of over-expansion posteriorly, More physiologic forces minimize trauma to cleft defect(s), Surgeon can perform fistula closure and bone graft WITH THE BRACES ON! This solves the dreaded relapse issue that we face when we have to remove expanders and place retainers to take the pt to surgery.
Doesn’t impact speech! Food doesn’t get caught in the cleft defect above the expander, Facilitates more normal/physiologic tongue function, Patient comfort!, More efficient for your practice – less chair time, fewer emergencies, etc.
The first 2000 days. This is the link to a 15 minute talk delivered by Dr Elizabeth Murhpy at a recent symposium in New South Wales, Australia. Her medical team includes a Speech Therapist and a Physiotherapist. She shows some very interesting graphs. I would like to see ENT, OMT and Osteopathy also included but it demonstrates an awareness of the benefit of collaboration. https://www.youtube.com/watch?v=BwYIV9JS4qs
Anthony Goldsmith, Rhythmic Movement Training International, located in Melbourne, Australia. I help children and adults unlock their full potential by addressing the root causes of developmental and movement challenges. Through targeted reflex integration, functional movement strategies, and a holistic approach to neurodevelopment, I support individuals in overcoming learning difficulties, sensory processing issues, and motor delays.
I work closely with families, educators, and other professionals to create customised programs that build lasting change. Whether it’s refining coordination, improving focus, or building resilience after trauma, my goal is to help every individual thrive. https://www.facebook.com/share/19MoEWM8FY/
Dr David McIntosh, Paediatric ENT, talks with Dr Derek Mahony about the importance of Early Intervention. https://www.facebook.com/ffomelbourne/videos/have-you-listened-to-our-podcast-episode-with-ent-dr-david-mcintosh-he-is-such-a/636401149455404
Dr. Kevin Boyd on ‘Geriatric Medicine in Pediatric Dentistry’ – podcast with Dr Simon Wong. https://youtu.be/4_8jLxNKzQ0
Dr Helen Jones – some case examples using a modified Biobloc Stage 1. Active treatment time approx.18 months.
Dr. Mike Mew’s moving tribute for his dear father: It is with great sadness that we announce that Professor John Mew passed away last week. He will be greatly missed but his vision, knowledge and deep understanding will be his lasting legacy.
https://www.youtube.com/watch?v=6lMK8lPhwGo
Dr Marianna Evans discusses the truth as it now is: Traditional orthodontics can no longer justify ignoring developing malocclusions and delaying treatment until the teenage years!!!
The DOC Podcast by Dr Mike DeLuke: In this episode, I welcome Dr. Kevin Boyd, a renowned pediatric dentist and expert in early orthodontic intervention, anthropology, and evolutionary oral medicine. Together, we explore the importance of early diagnosis and treatment of malocclusion, the interplay between genetics and environment, and the need for a paradigm shift in orthodontic education and practice.
Notable Quotes from Dr Kevin Boyd:
- “We are hardwired to have the capability of epigenetically producing a beautiful craniofacial structure-if we get the right environmental inputs.”
- “You don’t have to treat every child, but you do have to perform a validated risk assessment.”
- “It only takes one case to see the life-changing impact of early intervention.”
Dr Steven Lamberg introduces his Screening Tool for OSA& SDB – https://drlamberg.com/storage/app/media/2024/LQ_V16.pdf
Screening tool for OSA and other sleep-related breathing disorders can screen for signs and symptoms of SRBD Article in the Journal of Dental Sleep Practice.
Dr David McIntosh, Paediatric ENT, shows how “It’s All Connected!”.
Prof. John Mew’s last message: From Beyond the Veil
“If you’re hearing my words now, it means my time among you has passed. But ideas — the true ones — don’t die. They live on in minds that dare to question and in hearts brave enough to change.
I spent my life asking questions no one wanted to ask — and offering answers many were not ready to hear. I was not always welcomed. I was often misunderstood. But I never lost sight of the simple truth:
We are not born broken. We are shaped — by habit, by environment, by culture.
The face is not just a canvas of beauty; it is the map of your health, your development, your identity. How you breathe. How you hold your head. Where your tongue rests. These things matter — more than most will ever realize.
I challenged an entire profession not to criticize it, but to wake it up. Because orthodontics, as it stands, too often treats symptoms, not causes. And children suffer in silence when their growth is misunderstood.
To parents: start early. Guide gently. A child’s future — their airway, their posture, their confidence — lies in your hands.
To professionals: do not fear controversy. Fear complacency. The truth has never belonged to the majority, but to those willing to seek it, even when it’s uncomfortable.
And to the next generation: you are the guardians of a new way. Build a world where form follows function, and health begins not in treatment, but in understanding.
I may be gone from the world of flesh and breath, but my voice, my message, my hope — they remain. Let the face grow forward. Let the child grow free. Let truth grow louder than fear.”
The Global Summit Institute – Addressing the threat of Corporates, Insurance & AI in third party interference with the practitioner/patient relationship.
Video by Dr Soroush Zaghi MD demonstrating Mid-Tongue Restrictions. https://www.facebook.com/share/r/19AnHLAZTW
This is a podcast for everyone. What is happening to our children? Beth Lambert is a former healthcare consultant and teacher. She is the Executive Director of PEACE: Parents Ending America’s Childhood Epidemic, an organisation that educates the public about the epidemic. She is also the director of Documenting Hope and has written several books.
Ep. 48: Early Oral Motor Development: The Foundation for Speech, Breathing, & Health with Diane Bahr
Dr Jessica Waller, Myobrace provider explains how to carryout an initial patient screening: https://myoresearch.com/en-au/free-webinar-005 This is a very useful video for those who are new to assessing growth & function in the early years.
The Future of Dentistry:
AI,Ethical Practices and Global Standards: Dr Kianor Shah.
Mission & Vision Speech for Global Summit Institute: Dr Kianor Shah. on the occasion of the Award Ceremony, 12 June, in the Forte Village, Pula, Sardinia.
https://www.youtube.com/watch?v=iINNYbfWObI&t=181s
Dr. Mike DeLuke’s Orthotown Articles: Beyond OSA
-Part I: https://www.nxtbook.com/farran/orthotown/orthotown-march-2025/index.php?startpage=36#/p/34
-Part II: https://www.orthotown.com/magazine/article/9575/beyond-osapart-
Why now is the time to get involved in dental sleep medicine by Dr Aoife Brid Stack https://www.nature.com/articles/s41415-022-4944-9
In this DOC podcast Dr Mike DeLuke talks to Dr Piya Gandhi, a paediatric dentist in Houston. Dr Gandhi stresses the importance of screening by all health professionals and the application of the Fairest 6 Assessment. Also, how working collaboratively brings a greater understanding of other disciplines and their contribution to the wellbeing of young patients.
Here’s the link to the 12 free resources/articles that Dr. Boyd mentioned during the webinar we had with him on Monday which also included some fascinating research on optimizing our children’s health and lifespan:
https://drive.google.com/drive/folders/1jqgKXu7MbGvEFYin9nQP2obmIXtv3N6q
Links to the recordings of Dr Simon Wong & Dr Kevin Boyd’s webinars. Here’s the link to the 12 free resources/articles that Dr. Boyd mentioned during the webinar we had with him on Monday which also included some fascinating research on optimizing our children’s health and lifespan:
https://drive.google.com/drive/folders/1jqgKXu7MbGvEFYin9nQP2obmIXtv3N6q
In case you haven’t had a chance to watch it yet (or missed part of it), the full webinar is now available on our Youtube channel link below:
In this series, Professor Mew shares his pioneering work on Orthotropics, focusing on the crucial role of posture and tongue position in preventing malocclusion and guiding facial growth. His groundbreaking research challenges traditional orthodontics and he comes up with some very interesting facts.
https://www.youtube.com/watch?v=oMnP-iQL5HU
How the Trigeminal Nerve Affects Tongue Posture. http://www.instagram.com/reel/DHLsJEeO5XV/?igsh=MWFtMWRhMnQxbWxtZA%3D%3D
The Evidence basis for Early Interceptive Postural Orthodontics – Literature Review, Dr Simon Wong https://www.youtube.com/watch?v=KosbSjrIeH8
Dr Simon Wong’s 135 consecutive cases – Postural Orthodontics. Healthier Children Better Growth Straighter Teeth
Early Intervention Postural Orthodontics
https://naturalsmilescentre.com.au/#our-work__sec
Just click on this link to see the cases.
Statement by Dr David McIntosh, Paediatric ENT, about the importance of proactive care. I’m happy to categorically state that sleep disordered breathing is a medical condition characterised by some or all of mouth breathing, snoring, and apnoea is not normal in a child. Previously there have been suggestions that letting the child outgrow these problems was an acceptable form of care. For nearly 15 years now that suggestion has been found to be wrong, yet it persists in the mindset of healthcare providers. Given healthcare is such a large thing with many changes happening on a daily basis, it is impossible for anyone person to be across all of these changes. This is why it has become important for parents to be aware of this and the importance of proactive care.
With Dr Steven Lin: What is Airway and Myofunctional Orthodontics? – Dr Audrey Yun – MBC#38
Jan 9·The Mouth Brain Connection
Treating the Hot Air + Tongue Ties with Katrina Sandersabout:blank
The Beauty of Breathing by Airway Circle
Dr David McIntosh, paediatric ENT talks to CAFF host, Rebekah Downing, about Airway, Sleep & the Brain.
https://www.childrensairwayfirst.org/post/episode-13-of-airway-first
https://rss.com/podcasts/airwayfirst/985068/
David’s books include Sleep Disordered Breathing, A Parents’ Guide and Don’t Ignore the Snore.
Cochrane Library report:
Authors’ conclusions – see link to the full paper below.
There is no evidence from clinical trials to recommend or discourage any type of orthodontic treatment to correct Class II division 2 malocclusion in children. This situation seems unlikely to change as trials to evaluate the best management of Class II division 2 malocclusion are challenging to design and conduct due to low prevalence, difficulties with recruitment and ethical issues with randomisation.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005972.pub4/full#:~:text=malocclusion%20in%20children.-,Authors’%20conclusions,division%202%20malocclusion%20in%20children
This such a good podcast. EP:34 Breathe, Sleep, Thrive (w/Dr Shereen Lim)
the latest DOC podcast with Dr David Alfi, MaxFax.
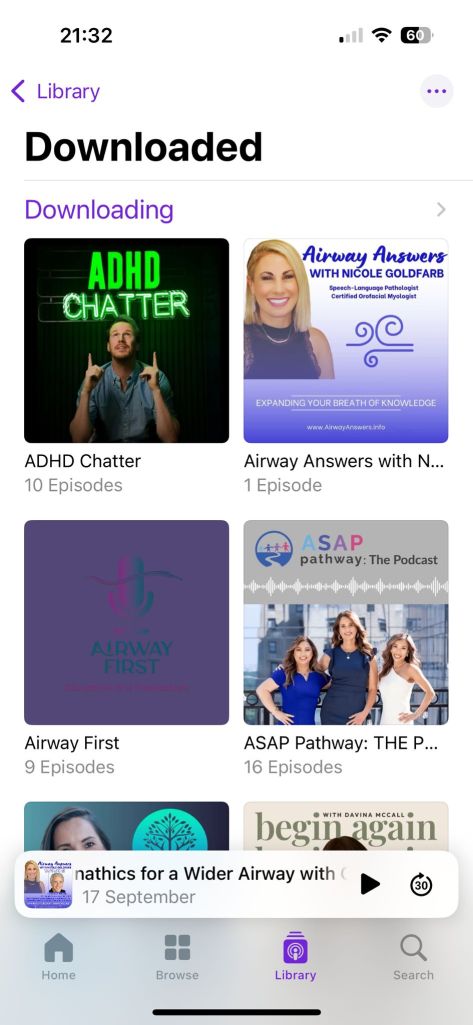
Children’s Airway First Foundation CAFF – multiple podcasts.
This is a really important podcast to watch. Dr Bill Hang explains so well all the principles which form the foundation of this society.
Children’s Airway First Foundation (CAFF) – conversation with Dr Claire Stagg
“ Smile – Everything Starts with the Mouth”.
Dr Stagg covers all the topics which this society encompasses.
This podcast about work/life balance should be of interest to all professionals.
Another not to be missed podcast! Dr Soroush Zaghi, explains the new paradigm for ENTs. https://www.sleepisaskill.com/podcasts/episode-170
Ask an Orthodontist: Dr Derek Mahony in conversation with Dr David McIntosh, ENT.
https://open.spotify.com/episode/63LRkDawpNyOhAZP6BRP0w?autoplay=true
See also: Ask an Orthodontist: Dr Derek Mahony in conversation with Prof. John Mew.
Do make time to listen to these podcasts with Dr Stacey Ochoa & Dr Mike Deluke on Early Orthodontic Intervention Part 1 & 2. ASAP pathway -A Platform to Help Your Child Grow Better. A platform to help parents identify the signs of sleep and airway disorders in their children.
Dr David McIntosh: The dental profession at large is very well aware of the need to be on the lookout for airway obstruction. A good research paper on the Airway/ Dental interface.
https://pubmed.ncbi.nlm.nih.gov/39061956/
Dr Shereen Lim, Perth, Australia, talks to Dr Stanley Lin, Maxillofacial Surgeon & ENT, California. The Palatal Expansion Controversy – Is there a role for orthodontics for better sleep & airway?https://www.facebook.com/reel/1067962977833820
CAFF (Children’s Airway First Foundation) Podcast: Dr Kevin Coppelson MD, DDS Oral Maxillofacial Surgeon working at the Breathe Institute, Los Angeles. His Dr Coppelson discusses his Minimal Invasive Nasal Dilation (MIND) surgical technique. His is an interdisciplinary approach, working with Dr Soroush Zaghi, ENT, Sleep Surgeon, and other health clinicians.
https://www.childrensairwayfirst.org/post/episode-74-of-airway-first
CAFF (Children’s Airway First Foundation) Podcast: Dr Hilary Pada https://www.childrensairwayfirst.org/post/episode-75-of-airway-first This is a truly amazing podcast and will be of interest to all our members. Do make time to listen/watch.
SDGF member Chris Harris DO Some thoughts from one particular Osteopath’s work in one particular very crucial area.
For many years on my training courses, I have many times heard the words “treat what you find”. I found this phrase rather vague and irritating; what the words are supposed to suggest is that, as a practitioner, you should be infinitely sensitive and adaptable as to what your patient’s body requires. For a long time, this sounded like a massive abrogation of responsibility to diagnose and fix. A cop-out in other words, and a mask for fluffy nonsense. Now I have changed my mind.
These days treating what I find is pretty much all I ever do. I hope to explain why and to give some insight
into osteopathic work as well. I am lucky to love my work: this is a precious thing which I cherish in my life. As a consequence, I find it fascinating, and I think about it a lot. Due to the contemplative nature of the cranial techniques, I have plenty of time to do this whilst working. Due to the time elapsed since my graduation – 30 years ago this month – my cogitations, if laid end to end, would go. . . well, quite a long way. Below I shall illustrate one of my central hypotheses. I’m not claiming it to be correct, but I do claim that this gives me comfort. My scientifically inclined intellect has always railed against the unknowable in subtle bodywork: “what on earth is going on” etcetera etcetera. I spend my days with my hands on people being given a veritable smorgasbord of information. Not all the time of course, but enough of the time to be useful. This can be about traumatic force vectors from car crashes, compressions from birth processes, infections in the past, emotional trauma, genetic abnormalities, and so on. Then bodies obligingly perform release and corrective processes while I observe. Again, not all the time, but enough to be useful. Quite what is going on while I do my detecting and patients do their rearranging nobody knows. This is something I find rather vague and irritating. I have however had my nose rubbed in indisputable, profound and excellent health changes repeatedly reported by my patients many times. So, I have to repeatedly tell my sceptical intellect to shut up so I can get on with the job.
During this process, in order not to feel too conflicted between the fluffy and the scientific I have to rationalise. I do this by hypothesising. Hypothesis no1. When we are interested in something we want to know more. So, we think about it, discuss it with other interested people, and study it. This is a kind of love, or at least empathy. So, with Osteopathy it is the anatomy that we get stuck right into – not just the toe bone connected to the foot bone. We enjoy imersing ourselves in the arcane detail: structure, function, histology, physiology, the evolutionary perspective, and, most complex and revealing of all, the embryology. This when internalised seems to act as a kind of scaffold for information to land onto, visible when we palpate and treat. When I attempt to explain what happens to patients, sometimes I use this analogy. Imagine if you will a friend you know well and who you care about. Imagine how the same friend would be if they were carrying a burdensome secret: probably distracted and out of sorts. You can sense this, and you want to help them, and you try to do so. The approach you make has to perfectly match what is required for the friend to feel safe enough to release what they need to. Arm round the shoulder, the right words and so on. The story gets told; they feel better. The scaffold of knowledge and experience I describe is what allows tissues to do the very same thing. The body seem to recognise your efforts and empathy, and then the tissues start to talk. They tell their stories and their burdensome secrets. I often get a sense that they are saying “Oh, bloody hell at last! Somebody who understands and who is actually listening. Phew!” The tissues express themselves by releasing, unwinding and decompressing. The patient feels better, thanks me, pays me money and goes away. All of which is nice: it’s a win-win. This idea works for me. Of course, the actual mechanism remains unknown. I would dearly love to see pointy headed scientists going around in lab coats carrying clipboards and measuring it all on big machines going ping ping. There will be a physics to it all but alas we are not there yet. One fine day I hope it will happen.
Maxillae talk to me. A lot. I find them very expressive and responsive. In fact, the whole mid face: the
vomer, palatines, the ethmoid and upper teeth all are relative chatterboxes. I am bemused by osteopaths
who purport to be cranial practitioners who say that they don’t work in the mouth. I find it ridiculous. This
area fairly shouts at me demanding attention when I palpate. Why does this happen? A clue lies in my own history. I had a difficult birth with the cord round my neck which left me with significant giocephaly. Likely as a result of this I had an obstinate finger sucking habit. My left index finger was white and wrinkly for the first eight years of my life and remains rotated away from my thumb by about 15 degrees. The idea from my tribe is that by doing this the child is subconsciously trying to release a compression. Debatable but possibly true. I pushed out my upper incisors so that they were proclined about 45degrees. My local dentist then rammed home the damage by extracting my upper 4’s and fitting a brace.
I remember waking in tears from the anaesthetic. My body knowing a wrong had been done perhaps.
Debatable again. Possibly true again. I hated the brace because it stopped me from sucking my finger,
abruptly halting the vain attempt to ameliorate my birth strain. Move on eight years. On the way to school I cycled at speed into the back of a neighbour’s car whilst looking down at my malfunctioning derailleur gears. The neighbour, a radiologist at Sevenoaks hospital, then had the job of x-raying my head. No fractures, not even much of a concussion but the nose swelled sufficiently that I could not look straight ahead. The central incisors slowly died over a decade or so. The nasal septum, buckled and blocking one nostril, had to be surgically corrected. This was not fun, especially when five feet of bloody gauze was removed. It made me think of Egyptian mummies having their unpreservable rapidly putrefying brains removed by hooks via the nostrils. So, my poor old face has had a bit to cope with. Osteopathically this is a big feature in my system and has caused my body problems. This is possibly why I was drawn to working in this area. The old cliche of physicians trying to treat their own problems via their patients. Debatable, possibly true. Anyway, I have practiced and treated and studied and made that internal scaffold. So, when I palpate the cranium of my patients, the middle of the face often tells stories. If I am to anthropomorphise the tissues, then these would be examples. “Crikey! My poor old mum should have had a C-section, for crying out loud! My infant head got a right squashing. Sphenoid, take a big breath in, and for goodness’ sake, stick those greater wing elbows out. Oooo that feels GOOD…” or “Get that bloody wire out from behind my upper canines NOW!! I have felt really rubbish for bloody YEARS. What idiot put that there?!” or, with my own brother, memorably the following: “Yes, yes, of COURSE you can release the compressed sacro-coccygeal articulation and relieve the pain that started when this overweight body fell asleep slumped in a plane seat six months ago. For a few days. Big deal. But it keeps on quickly reinstating itself. Of course, it bloody does because you haven’t looked at the jammed-up ethmoid. C’mon! You know the whole dural system is functionally connected by its
attachments at the caudal end balancing movement via the falx’s anterior end at the crysta galli. For
goodness’s sake you’ve even been to the practice called the crysta galli for treatment by your teacher.
Remember?! So, release it you silly bugger!” I did, using an intra oral technique in order to mobilise the
vomer: jammed ethmoid equals jammed vomer and vice versa. My beloved chubby brother abruptly
achieved lasting relief from his painful coccyx.
Seriously, I find that there is a lot to do in the midface and there are good changes as a result. I get to work and get the maxillae moving. I release the articulations around the vomer and the palatines plus between these structures and the sphenoid. I feel into the rude jostling between individual teeth along a crowded arch. Sometimes you can detect undescended teeth butting up against descended ones. The space you make is a little like applying WD40: canines descend when dentally it doesn’t look likely. Also, there are compressions held intraoseously. As in not between the bones but within them, often from birth strains or lack of stimulation due to truncated or absent breastfeeding. These are at the root of a lot of poor arch development, and it is possible to release these. Do this, then through the wonderful omnipresent mechanism of osteoclastic and osteoblastic remodelling there will then be a shape change: make more space and the bones will grow. Not just in growing patients but in adults as well. Here is one example: One patient had been knocked flying by an impact from a football into her face at age 15. I released this age 25.
Within a few days three of the upper incisors had changed their orientation by about 20 degrees. Two
forward and one back. She was not happy about the snagglyness on an aesthetic level, but she was happy
about the changes to her pituitary function. The impact’s forces had gone deep into the skull and distorted the little gland’s home within the Sella Turcica. When the Pituitary is not happy, the hormones will not be happy. She had been unable to control her temper for three days a month before her period. Most gratifyingly this then settled. As I have mentioned, insights into embryological timelines and processes are something that tissues love. The sutural seam that joins up usually prenatally between the pre and postmaxilla is a lively area to treat. In treatment, I hold canines or tuck in for a contact behind the lateral incisors and feel back along the suture’s length. It displays all sorts of shears, buckling and distortions, all gasping for release. Because it has more flexibility than the rest of the bone if there is a compression, it will frequently show itself there. Dentists will recognise the morphological consequences of this, I am sure. Xrays may not show this functional axis, but it shows itself on palpation. So, we get the strains released. Not just the sutures, but into the bony matrix. The ‘Full Monty’, as in when you want maximum deep-seated change, is when you engage factors such as the issues displayed by this suture. Do a good fulsome job and you can feel the bones expand and increase vitality under your hands. It feels like they are taking a big breath in. Hence the silly-to-some sounding idea that the bones breathe. It certainly feels like it to me anyway. When this kind of release occurs in an underdeveloped maxilla, there will be a growth spurt both sagitally and laterally. If done in conjunction with dental orthopaedic arch development, then the rule of thumb is that the rate of change will be roughly doubled, whilst unwanted secondary effects are minimised.
So, back to the first comment. Treat what I find? These days yes, I absolutely do. I listen to the body. The body feels my experiences and talks back. Especially the face, most especially the maxillae. I go with this and do my best to listen to the best of my abilities. Not just because it feels easy and natural, but also because I know for damn sure that to get the face working is important. All this from my osteopathic training and also from the wonderful interchange of information I have had over the last twenty years with my dental colleagues. People who have had to be imaginative and brave in the face of much opposition. I am very happy to be part of this gang, so thank you and thank you for reading this. It has been a long-held dream to demonstrate some of what I have talked about with a good study: anyone interested? I’m terrified of the academic formality that would be involved, but I would be happy to have my hand held. It would just need perhaps three treatments before any ortho work and some scans before and after. This I think would be a world first. If it was demonstrated that bones could grow differently in response to a trained pair of hands, let alone with the aid of an ALF, it would absolutely help our cause. I am completely sure of this.
Dr Michael DeLuke talks with Dr Kevin Boyd. 25 July 2024 Episode 62.
Don’t miss this episode with the amazing Dr. Kevin Boyd! Kevin is a world-renowned expert in the area of early orthodontic treatment and we had a fascinating discussion on if, when, and why to provide orthodontic treatment to younger children.
Dr Sharon Moore interviews Dr Marianna Evans, dual qualified periodontist-orthodontist.
https://www.facebook.com/reel/1267200130913468 cut & paste for an amazing interview.
Member of the Society for Dentofacial Growth & Function (SDGF), Dr Steffen Deker talks with Dr Michael DeLuke. Episode 58

C-GASP Level 1 Screener Registration – Message from Dr David McIntosh ENT, PhD.
Children’s General Airway Screening Protocol (C-GASP). Developed by the
Children’s Airway Screener Taskforce (CAST) sanctioned by the ADA to create a screening protocol for pediatric OSA.
Attention USA!
This is a really big and important opportunity to become involved in screening children and adolescents for upper airway obstruction. Already several hundred of patients have been screened and we want this to become hundreds of thousands.
This project is sanctioned by the ADA and is a great initiative to make dental clinics an important sentry to find kids not breathing and sleeping properly. So please- register your clinic! It’s totally free of cost to be part of this project. And tell them I sent you!
Anywhere else in the world- you are very much welcome to register too. Whilst not exclusive to dental clinics, certain measurements and data are more geared towards having some dental knowledge but if you’re enthusiastic that’s enough to get you on board too!
https://airwayassessment.azurewebsites.net/register
John Flutter – “John Mew’s Tropic Premise“
The ideal development of the jaws and teeth is dependent on correct oral posture with the tongue resting on the palate, the lips sealed and the teeth in light contact for between four and eight hours a day. For that to occur the child must be breathing through the nose all the time. Most children have their mouth’s open most of the time.
As a result of this the tongue falls from the roof of the mouth. The oral seal is lost and the child is then breathing through the mouth. The tongue and the mandible are a single anatomical unit, when the tongue falls down and back the mandible does also. Without the tongue to support the maxillae and promote its forward growth the maxillae grow in a more down and backward direction with inadequate forward growth.
The mandible grows downwards and backwards resulting in at the gonial angle increasing. As the mandible drops down and back it impinges on the airway and the head is tilted back. to maintain adequate pharyngeal airway. The forward head posture is often compensated by increase lordosis or curvature in the spine, often with rotated pelvis. When the tongue is resting in the palate as the tropic premise suggests the upper teeth erupt around the tongue forming a well developed upper arch and well aligned upper teeth. When the upper front teeth are crowded as a result of poor tongue posture the nasal passages will be restricted by the same amount.
When the upper arch has not developed sufficiently forwards the pharyngeal airway is restricted. When the maxillae are distorted every bone in the cranium will respond and will also all be distorted. This distortion leads to many cranially related neurological problems. When the maxillae are down and back and the mandible has swung down and back under it there will be general restriction of the jaw joint leading to Jaw Joint problems. The maxillae down and back is related to sleep related breathing disorders.
When a child is mouth breathing especially while sleeping they have increased breathing rate and greater tidal volume. These features mimic an adrenaline response. The child will will be in a sympathetic mode as if they are stressed. They are in this condition most of the time. This itself leads to stress and further exacerbates the problem. When an individual is under stress the the body’s natural immunity capacity is reduced. The solution is simple, the implementation of the solution requires radical changes. The solution is mostly educational. We need to educate both parents and children. We need to deliver a programme to help children keep their lips together and the tongue in the roof of the mouth. Once we accept this is an educational challenge more than a clinical challenge the better the results will be. I have experience in creating educational programmes to deliver this in such as way as to be affordable for families but at the same time profitable for the practice. I have done this in dental practices only.
Mike Mew – ” Cranial Dystrophy”
A possible pathological process underlying malocclusion, which relates malocclusion with a range of other diseases and problems”. The common aetiology is the tongue falling from the roof of the mouth in order to ventilate the lungs via the mouth, maybe using the nose as well in some instances. Most children have their mouths open most of the time. There is proper research to support this if you cannot verify it yourself every day with your own eyes when you see children. The medical profession and ENT’s regard mouth open posture as normal and say children usually grow out of it. That is true but by then the damage has been done the maxillae are down and back and the entire airway is compromised and all the cranial bones are distorted.
The really important point and in my view not understood is that the mandible and the tongue are a single anatomical unit. When the mouth falls open the tongue follows it down. Conversely in therapy when the tongue is moved up and forwards into its correct position it takes the mandible with it. When seen like this it is more apparent. Once the tongue falls from the roof of the mouth the maxillae neither develop adequately transversely or do they grow and develop sufficiently forwards. This leads to restrictions in the pharyngeal and nasal airways. It leads to every bone in the cranium being distorted. Cranial neurology is affected by the distorted cranial bones. Head posture is altered to maintain airway compensation takes place through the entire skeletal structure to maintain balance of the head in a forward position. The head is heavy and it needs to be balanced.